Professor: This post will finish the proposed six (6) stages for handling breathing discomfort. So far, we have completed a tour through the first five (5) stages:
1. CONTACT! A breathing alarm signal just arrived at posterior insula!
2. SEND OUT ALERT! Anterior insula and the rest of saliency network (SN) received the alarm, too!
3. FULL ATTENTION! The SN puts the Central Executive Network on the lookout & quiets down the Default Mode Network!
4. GET READY TO ACT! Task: Breathing 'tubes' want medication via inhaler!
5. ACT! Action: Go get inhaler and use it!
Professor: We will add a final, sixth stage for communication to Menon & Uddin’s model of five perceptual processing stages (2010) that has been our guide for the first two parts. (Here are links to Part 1 and to Part 2.)
6. COMMUNICATE! Let others know how well the medication is working!
Professor: This sixth stage includes listening for the meaning of a question and then answering it. For us, the answer will estimate a subjective rating of shortness of breath. For example, “Easy breathing” or “It’s moderately hard to breathe!”
Student: Some people ask me about my breathing. And I really don’t know what to say!
Professor: Asking questions is great tool for opening our ability to connect to our self. Already our mind has shifted its attention and is taking actions. Talking about symptoms, while experiencing them, is in the details for the upcoming Stage 6: Communicate!
‘Sound to Meaning’ – Semantic Processing of Sentences
(Editor – for a discussion of ‘Sound to Meaning’ sections on word form processing and syntactic processing of sentences, please click this link.)
Professor: Let’s look at how well organized a sentence may be.
- If it is well-formed, then all the rules of syntax are obeyed and it ‘flows’ easily.
- However, if the sentence is, “I just ate a cloud.” it might ‘flow’ easily, but it is ill-fitting with one’s knowledge of the world” (Pylkkänen et al., 2011).
Student: Then, how does my ‘language mind’ know if the well-formed question, “What is your dyspnea number now?” is also well-fitting?
Professor: Based upon their elegant experiments on sentences, Brennan and Pylkkänen (2010) suggested that the primary loci for basic combinatorial processing are the
- ventromedial Prefrontal Cortex for deciding the most likely semantic structure and the
- left anterior Temporal Lobe for reconstructing the inferred syntactic structure.
Student: Now let’s ‘find’ the meaning of our sentence, “What is your dyspnea number now?”
Professor: Its meaning may become more understandable as its words are processed, perhaps as shown in the table below:
| Word | Meaning | Sound Stress |
| What | it's a question => 'tell me about' | Higher |
| + is | 'something equals something' | Lower |
| + your | 'my' | Also low |
| + dyspnea | 'uncomfortable breathing' | Highest |
| + number | 'intensity' | Low |
| + now | 'at this time' | Higher |
| All together | Tell me a number for your uncomfortable breathing. |
Professor: Listening just clued us that we heard a question, that is a request to choose a dyspnea scale descriptor, take its number, and then say the number out loud.
Sound to Action
(Editor – for a detailed discussion of ‘Sound to Action’ sections on magnitude estimation and inner speech construction and auditory production of sentences, please click this link.)
Professor: The flip-side of listening is answering. Since our question is, “What’s your dyspnea number now?”, then the answer could be, “My dyspnea number is […].”
Professor: Let me check what my thinking and speaking actions might be to estimate the magnitude of my own sensations for being short-of-breath (SOB):
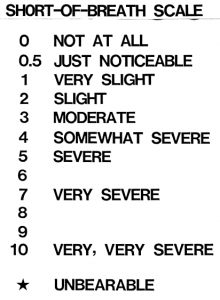
- I ‘see’ the 10 point scale (Borg, 1982, 1998) in my mind’s ‘eye’ even though it is hanging in front of me and choose ‘severe’ SOB that has a scale number of “5.”
- Now I use my articulatory motor system to say “5″ out loud.
Student: And as a scientist, how did your brain estimate SOB magnitude?
Magnitude Estimation
Professor: That’s quite a very provocative question. Think of a burner on a stove and putting your hand high over it. Your hand might feel somewhat warm, and as I turn up the burner heat, you could say that, “Now the skin on my palm is beginning to feel very warm. In fact, I am pulling my hand away.” You just used magnitude estimation!
Student: But how do you estimate the magnitude for this thermal challenge and also for dyspnea attacks?
Professor: Surprisingly, pain and dyspnea activate mostly the same cortical networks.
- Von Leopoldt and co-workers (2009) found that the discomfort from dyspnea and from thermal pain activate common human brain network, and
- this brain activity seems to correspond to Stages 1 and 2 for the sensation processing model of Menon and Uddin (2010).
Student: Therefore, this is a ‘conserved’ Searchlight function of the posterior insula. But how do we ESTIMATE MAGNITUDE?
Professor: Well, the mechanism for MAGNITUDE ESTIMATION is a bit of a mystery for me. A well-designed experiment done by Baliki et al. (2009) will provide some clarification.
- The subjects rated thermal pain during a fMRI scan using a finger-span device;
o the investigators created lines on slides having the same length as each of the subjects’ thermal ratings.
- The subjects rated these visual lengths during a separate scan,
o which were varying in length unbeknown to them as did their heat pain ratings.
Professor: Of course, these investigators wanted to know how variable were the ratings for each subject; that is,
- how much magnitude variability there was in a participant’s ratings; so they
o calculated the variance for the pain ratings and for the visual length ratings.
- Note the experimental design assured that the average variance of pain and length ratings would be similar,
o since the length rating was ‘a rating of the pain rating.’
Professor: Then they performed a whole-brain, voxel-wise, conjunction analysis
- to find areas that shared the same patterns of the mode-independent variance in ratings and found associated activity in
o specific areas of the bilateral insula that were for magnitude only, that they termed mag-INS.
Professor: Lastly Baliki and co-workers performed a contrast analysis to compare the pain- to visual-task modal ratings with the ROIs that encoded pain task variance and
- found that the pain-specific activity was found in
o altogether different areas of the bilateral insula, that they termed noci-INS.
Student: Wow! They struck GOLD!
- The mag-INS areas estimates and stores the magnitude of the pain sensation whereas
- the noci-INS areas are telling us that
o significant pain is happening and perhaps is specific enough
o to indicate it is being detected by the inspiratory muscle and lung tissue receptors.
Professor: Yes, now that we are sensing the role of the mag-INS in intensity estimation of thermal pain, let’s try to answer the bigger question, “How does one get the dyspnea scale score number and then say it out loud?”
Student: In fact, I was thinking that I should use my inhaler before I go running.
Professor: Well, using the modified Borg SOB scale (shown below; Weiser et al. , 1993), what is your dyspnea descriptor and number now?
Student: My SOB is ‘Somewhat severe’ which is a score of ‘4.’ Yes, it’s time to use my inhaler. Say, isn’t this a cognitive task that uses inner speech!
Professor: Yes, it sure is.
- That means it is essentially a covert process that is referenced to the self, for choosing a number (i.e., covert language) to later say out loud (i.e., overt language).
- It is waking thought as opposed to dreaming thought, or even ‘day dreaming’ thought (Carter & Furst, 2010).
- Some experts and lay people call this
o inner speech, private speech, or, as I prefer, self-talk.
Student: Okay, I have taken two puffs from my inhaler. I can exhale a bit better. So how do I find a new number for my SOB rating?
Professor: Let me make up a play. First we must have cortical areas as actors and actresses. Below is a listing. (For each area, see either figure 3 from Von Leopoldt and co-workers (2009) or figure 1 from Specht, 2014 or see expanded discussion):
- dlPFT (dorsolateral prefrontal cortex, to left of ventral Premotor Cortex, from Specht)
- SMG (supramarginal gyrus, from Specht)
- INS (insula, from Von Leopoldt et al.)
- IPS (intraparietal sulcus, just above SMG, from Specht)
- pMTG (posterior middle temporal gyrus, from Specht)
- vPMC (ventral premotor cortex, from Specht)
- PreC (precentral (motor) cortex, from Specht)
- dACC (dorsal anterior cingulate cortex, from Von Leopoldt et al.)
- IFG pOp (inferior frontal gyrus, pars opercularis, from Specht)
Professor: However, I am not sure whether our brain uses a dialogue format; if it did, the script for a conversation might go like this:
Professor: However, I am not sure whether our brain uses a dialogue format; if it did, the script for a conversation might go like this:
- Get the current SOB state:
dlPFT to INS: “What’s a scan of my breathing feel like now?”
INS to dlPFT : “Your body is a bit short-of-breath.”
- Get current SOB scale descriptor and number:
dlPFT to SMG: “I have instructions for you to look at your copy of the Borg scale.”
SMG to dlPFT : “Last time your rating was ‘Somewhat severe’ with a number of ‘4.’”
dlPFT to SMG: “Please help IN estimate the present SOB intensity for us.”SMG to INS: “Does SOB feel like ‘somewhat severe’?”
INS to SMG: “No. It’s not that intense.”SMG to INS: “How about ‘moderate’?”
INS to SMG: “No. That’s still too intense.”SMG to INS: “Do you feel you have ‘slight’ SOB?”
INS to SMG: “Yes. It’s just ‘slight’.”
- Verify SOB scale descriptor and its number:
SMG to INS: “So, after using the inhaler, your SOB descriptor of ‘slight’ with a number of ‘2’ fits okay?
INS to SMG: “Yes.” - Announce the SOB scale number:
SMG to dlPFT : “The SOB score for ‘slight’ is ‘2.’”
- Get word for SOB scale number:
dlPFT to IPS: “What’s the word for ‘2’?”
IPS to dlPFT : “The non-symbolic label is ‘TWO'”.
- Assembly phonemes for SOB scale number:
dlPFT to IF and pMTG: “Please get the individual phonemes for the word ‘TWO.'”
IF and pMTG to dlPFT : “These phonemes ‘| tu: |’ are now in the auditory working memory.”
dlPFT to vPMC: “Now prepare an articulatory motor plan for saying ‘| tu: |.’
- Say phonemes for SOB scale number out loud:
vPMC to PreC: “Give the GO signal to execute the motor plan for ‘| tu: |’!”
PreC: “Okay you special articulatory motor units for voicing ‘| tu: |.’
– GET READY TO SAY ‘| tu: |’ LOUDLY;
– SET;
– GO!” - Get self-feedback while speaking:
dlPFT to INS and dACC: “Any errors or corrections from PreC’s ‘GO’ signal?”
INS to dACC: “No interoceptive mismatches; prosody and emotional tone are appropriate!”
dACC to INS: “Then, no corrections have to be made!”
INS and dACC to dlPFT : “We agree! No errors; no corrections!”
dlPFT to ALL: “Well done!
Professor: Maybe that dialogue happened; maybe it didn’t. But, surely something like that happened.
Student: Hmm. I do a lot of ruminating, and your dialogue sounds very familiar to me.
Professor: Thanks. This is the end of the last stage, “Communicate!,” which basically
- first, consisted of a question requesting current SOB scale number and
- second, provided a verbal answer by
o estimating the intensity of breathing discomfort (in this case),
o matching it with an item on a discomfort rating scale,
o retrieving the item number from long-term memory, and
o saying the number out loud.
Conclusion
Professor: Now we have come full circle from Part 1. All stages are listed below in the Take Home section.
And I am looking forward to applying these six stages to other sensations, for example, to perceived exertion and to physical fatigue.
Take Home: Six stages of processing perceptions:
| 1 | ALARM IS SOUNDING! | A breathing alarm signal just arrived at posterior insula! |
| 2 | SEND OUT ALERT! | Anterior insula and the rest of saliency network (SN) received the alarm too! |
| 3 | FULL TASK ATTENTION! | The SN starts the Central Executive Network processing situation & quiets down the 'chatty' Default Mode Network. |
| 4 | GET READY TO ACT! | Task preparation: Breathing 'tubes' want medication via inhaler. |
| 5 | ACT! | Action: Go get inhaler and use it! |
| 6 | COMMUNICATE! | Others want to know how well the medication is working! |
Coming up next: What is Perceived Exertion? Can these six stages for processing perceptions be applied to producing effort and to estimating effort.
References
Baliki MN, Geha PY, Apkarian AV. Parsing pain perception between nociceptive representation and magnitude estimation. J Neurophysiol 101: 875–887, 2009. DOI:10.1152/jn.91100.2008.
Borg, G. (1982) Psychophysical basis bases of exertion. Med Sci Sports Med 14: 377-381.
Borg, G. (1998) Borg’s Perceived Exertion and Pain Scales. Champain, IL: Human Kinetics.
Brennan J, Pylkkänen L. (2012) The time-course and spatial distribution of brain activity associated with sentence processing. NeuroImage 60: 1139–1148. DOI:10.1016/j.neuroimage.2012.01.030.
Carter R, Frith C. (2010) Mapping the Mind. Oakland, CA: University of California Press.
Menon V, Uddin UQ. (2010) Saliency, switching, attention, and control: A network model of insula function. Brain Struct Funct 214: 655–667. doi:10.1007/s00429-010-0262-0.
Pylkkänen L, Brennan J, Bemis DK. Grounding the cognitive neuroscience of semantics in linguistic theory. Language and Cognitive Processes 26: 1317-1337, DOI: 10.1080/01690965.2010.527490.
Specht K. (2014) Neuronal basis of speech comprehension. Hearing Research 307: 121.135. DOI.org/10.1016/j.heares.2013.09.011.)
von Leopoldt A, Sommer T, Kegat S, Baumann HJ, Klose H, Dahme B, Büchel C. (2009) Dyspnea and pain share emotion-related brain network. NeuroImage 48: 200–206. doi:10.1016/j.neuroimage.2009.06.015.
Weiser PC, Mahler DA, Ryan KP, Hill KL, Greenspon LW. Clinical assessment and management of dyspnea. In: Pulmonary rehabilitation: Guidelines to success. Hodgkin, J, Bell CW, eds. Philadelphia: Lippincott 1993, 478-511.
9 July 2014
This post has been revised by
• condensing the original to emphasize Semantic Analysis of “What’s your dyspnea scale score now?”,
• discussing Magnitude Estimation by posterior insula,
• showing the imagined cortical dialogue to get and talk out the answer, “2”, and
• concluding with a summary of the Six Sensory Processing Stages.